Food allergies, intolerances, and sensitivities are increasingly common. You’ve heard of nut-free schools and gluten-free foods, and yes, some people truly need to avoid even the tiniest traces of these foods. In fact, millions of Americans experience allergic reactions to foods every year. While most reactions are mild, some can be life-threatening and require emergency treatment or hospitalization.
How do we know whether our symptoms are from an allergy, intolerance or sensitivity? Where do they come from, and where does celiac disease fit in? What are the best ways to prevent, treat, and live with them? Keep reading to find all of the essential answers in this blog post.
Food Allergies
Food allergies are an abnormal response to food that’s triggered by the immune system (the system that fights infections). It happens when the immune system mistakes a non-harmful food, like peanuts for example, for a serious invader and overreacts to it. The immune system creates a specific type of compound called an IgE antibody that is responsible for most of the symptoms of true allergies. These IgE-mediated allergic reactions can be non-serious or serious and life-threatening. Symptoms are immediate and include skin rashes, tongue swelling, nausea and vomiting, shortness of breath and/or anaphylaxis.
Food Sensitivities
Sensitivities, on the other hand, are not life-threatening but can still be very uncomfortable and frustrating. The immune system creates an IgG immune reaction and symptoms are delayed, sometimes up to days later, making them difficult to pinpoint. Common symptoms of food sensitivities include bloating, gas, diarrhea/constipation, migraines, joint pain, brain fog and skin rashes.
Food Intolerances
Food intolerance is the inability to process or digest certain foods. The most common one is…you guessed it, lactose intolerance. Experts estimate that up to 70% of the world’s population has lactose intolerance. Lactose is a sugar found in milk that can cause gas to build up in the GI tract. This is not an allergy, but rather an inability to effectively digest it. Lactose is a two-part sugar molecule that needs the enzyme lactase to break it down. When someone does not have enough active lactase in their digestive tract, lactose remains intact and causes abdominal pain, nausea, excess gas, bloating, and diarrhea. Both food intolerances and sensitivities are dose dependent, which means that small amounts sometimes have little to no effect compared to larger quantities consumed.
Celiac Disease
Celiac, a digestive and autoimmune disease, is triggered by consuming gluten which over time causes damage in the small intestine. Gluten is a protein found in wheat, rye, and barley. According to the Celiac Foundation, it is estimated to affect 1 in 100 people worldwide and is hereditary. Since there is currently no cure for celiac, strictly avoiding all gluten is essential to heal the intestinal lining and avoid serious complications such as malabsorption, failure to thrive and delayed puberty in children, and infertility/miscarriages .
Where do allergies and sensitivities come from?
It’s unclear exactly where food allergies come from. Research shows that they could partly be genetic. Gut microbiota may also influence your chance of developing food allergies.
Unfortunately, there is no known cure for food allergies but reactions can be prevented. In an allergic reaction, the production of IgE antibodies is triggered by a protein in the offending food. Any food has the potential to cause an allergic response, however, there is a short list of foods that account for most reactions. These common food allergens must be declared on package labels, according to the FDA. Common food allergens include:
● Peanuts
● Tree nuts (e.g., almonds, walnuts, pecans)
● Fish (e.g., cod, bass, flounder)
● Shellfish (e.g., crab, lobster, shrimp)
● Eggs
● Milk
● Wheat
● Soy
Common food sensitivities also make up this list, but can include hundreds more along with food chemicals. Having an immune reaction to different, typically healthy foods is NOT normal, and most of the time stems from gut permeability, or leaky gut. There are tight junctions in our intestinal lining that keep our digested food inside the gut, where they belong. However over time things like stress, medications, bacterial overgrowth, inflammatory foods, and environmental toxins can cause these junctions to open up, allowing food proteins to seep into the bloodstream, where they absolutely DO NOT belong. This creates a cascade of inflammation throughout the body and leads to the symptoms mentioned above.
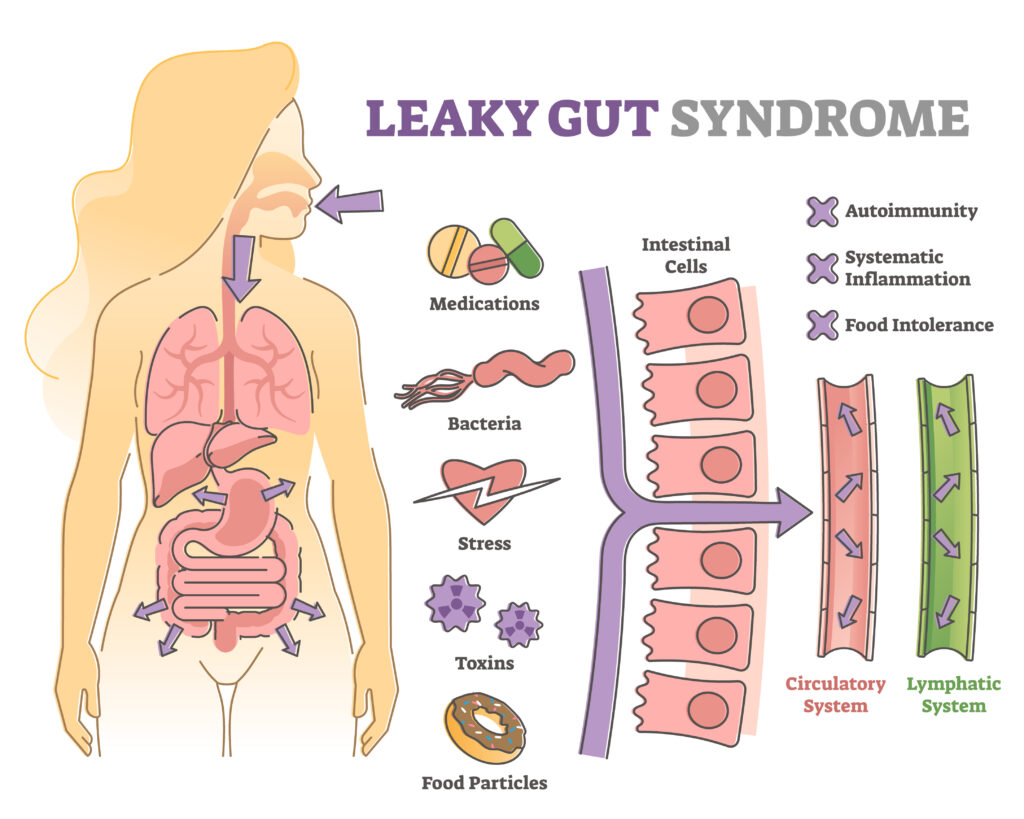
Identifying the foods that are causing inflammation is one of the first things to focus on, but can be tricky since symptoms can be delayed. Keeping a food and symptoms journal is a good place to start. Two of the most common food sensitivities that I see in working with clients is gluten and dairy. The proteins in gluten, in particular, can cause the gut cells to release zonulin, a protein that regulates tight junctions. Too much zonulin can cause the breakdown of these junctions in people who are sensitive.
Should everyone go dairy and gluten-free? No, but if you are unable to identify specific trigger foods through dietary recall, or we don’t test for sensitivities, it’s worth trying to eliminate them for 2-3 weeks to see if your symptoms improve. If so, then we add back in one food item at a time, slowly, so we can pinpoint the culprits.
Just removing the foods you are sensitive to, however, isn’t necessarily addressing the root cause of the problem. We need to work on healing the intestinal lining so inflammation decreases and the junctions are resealed. Eating a whole-food diet rich in plants, collagen, and healthy fats such as omega-3’s is key, along with addressing possible bacterial overgrowth and adding in targeted supplements to help nourish the lining creates an environment where your digestion can thrive.
Living with food allergies and sensitivities
The best way to deal with food allergies, intolerances and sensitivities is to avoid those foods that cause reactions for you. Here are my best strategies to deal with them.
- Read your food labels carefully. To help you avoid foods that you react to, most pre-packaged foods must clearly identify if they contain any of the major food allergens (or contain the immune-triggering protein of the major food allergens). Look at the list of ingredients, “allergen free” claims, and also for statements like “may contain” or “produced in a facility that also uses.”
- Wash your hands, surfaces, dishes, and utensils well to prevent accidental cross-contamination between offending foods and other foods for allergies and celiac disease.
- If you’re eating out, confirm whether the meal is free from the food you’re allergic or sensitive to before placing your order.
- Food allergens may also be added to certain medications and cosmetics, so check those labels or ask your pharmacist before purchasing.
- If you have had a serious anaphylactic reaction, it’s important to carry an epinephrine auto-injector in case of accidental exposure. This is a lifesaving medication that can help maintain your blood pressure and restore your ability to breathe. You can ask your pharmacist whether a prescription from a medical doctor is needed. Be sure to learn how to use it properly and replace it as it reaches the expiry date.
- Anaphylaxis is a condition where you may consider wearing a medical alert bracelet or necklace.
- For lactose intolerance, all milk products do not need to be strictly avoided, provided they are consumed with the lactase enzyme (available as a dietary supplement) or have been pre-treated with the lactase enzyme (e.g., lactose-free milk). These ensure that the lactose has already been broken down for you and should not cause symptoms of intolerance.
- If you believe that you may have a food allergy, discuss this with your healthcare provider. Navigating food sensitivities can be particularly challenging. I can help create a personalized plan for you, including ordering testing to help take out the guesswork.
- Eat real, whole foods vs. processed foods. Processed, packaged foods can contain a lot of hidden ingredients, in addition to added sugar, that you could be sensitive to. Switching to an eating plan that includes mostly foods that came from nature will not only make it easier to avoid food sensitivities, allergies, and intolerances, but it will provide the vitamins, minerals, digestive enzymes, and antioxidants that our bodies need to run optimally.
- Work on healing your gut. As mentioned above, this is key in helping you address food sensitivities. A lot of my clients are eventually able to add these foods back in over time!
- Decrease stress. Chronic stress increases a hormone called cortisol, which can affect digestion and lead to leaky gut. Start with slowing down when you’re eating. Turn off distractions if you can, and take a few deep breaths before taking your first bite. This will signal to your body that you are relaxing, which improves motility and absorption of nutrients.
If all of this sounds great but overwhelming, download my free Beat the Bloat 6-Day Meal Plan and E-Guide here.
Final Thoughts
Food allergies and sensitivities are increasingly common. There are several different kinds and most are not serious or life-threatening, however, they all cause unwelcome symptoms. As a general rule, avoiding the offending foods is highly recommended. This post contains several essential tips on how to live with food allergies and sensitivities.
If you believe you have a serious food allergy, it’s critical that you see your healthcare provider to determine if you need to carry emergency medication for future exposures.
For a customized plan designed to help you enjoy the meals you love minus the few foods that you may be allergic or sensitive to, consult a registered dietitian who can provide personalized research-based nutrition advice for your health, lifestyle, and goals. I can help. Here is the link to book a chat about making sure to meet your dietary needs and create a roadmap towards improving your symptoms!
References
Mayo Clinic. (n.d.). Lactose intolerance. Retrieved from https://www.mayoclinic.org/diseases-conditions/lactose-intolerance/symptoms-causes/syc-20374232
MedlinePlus. (2020, September 28). Anaphylaxis. Retrieved from https://medlineplus.gov/anaphylaxis.html
MedlinePlus. (2020, September 28). Food allergy. Retrieved from https://medlineplus.gov/foodallergy.html
Medscape. (2020, February 5). Food Allergies. Retrieved from https://emedicine.medscape.com/article/135959-overview#showall
National Institute of Allergy and Infectious Diseases. (2018, October 26). Identifying Causes of Food Allergy & Assessing Strategies for Prevention. Retrieved from https://www.niaid.nih.gov/diseases-conditions/food-allergy-causes-prevention
National Institute of Allergy and Infectious Diseases. (2019, September 11). Treatment for Living With Food Allergy. Retrieved from https://www.niaid.nih.gov/diseases-conditions/treatment-living-food-allergy
National Institute of Allergy and Infectious Diseases. (2018, October 25). Characterizing Food Allergy & Addressing Related Disorders. Retrieved from https://www.niaid.nih.gov/diseases-conditions/food-allergy-characterizing
NIH News in Health. (2017, March). Understanding Food Allergies. Retrieved from https://newsinhealth.nih.gov/2017/03/understanding-food-allergies United States Food and Drug Administration. (2018, September 26). What You Need to Know about Food Allergies. Retrieved from https://www.fda.gov/food/buy-store-serve-safe-food/what-you-need-know-about-food-allergies
